In the medical literature, there are more than 100 types of arthritis, which affect all age groups including children before the age of 10. Arthritis is defined as inflammation of the joint and the symptoms are swelling, stiffness, redness, pain, warmth and difficulty on moving the joint. There is also some arthritis whose symptoms are “non-inflammatory” such as osteoarthritis, which is still very much regarded as degenerative arthritis.

a) Rheumatoid Arthritis (RA)
If one has done a health screening package, hidden in the midst of an array of blood tests such as cholesterol levels, haemoglobin level, kidney function is a test known as Rheumatoid Factor (RF). Most results give either a positive or negative value but some do have the exact values which can be compared with the reference range. As its name suggests, a positive RF may be related to rheumatoid arthritis (RA). Of all the different forms of arthritis, RA is the most common inflammatory arthritis with a prevalence of rate of approximately 1%. Women are nearly three times more likely than men to develop this disease. The classical features are pain, stiffness and swelling of the finger and wrist joints.
RA affects both sides of the body in a symmetrical pattern. Larger joints such as shoulder, elbow, knee, neck can also be affected. It usually comes insidiously, over days or weeks and one usually does not able to pin-point the exact date of its occurrence. Most patients will complain of excessive stiffness of the fingers which improves as the day goes by. If left untreated, RA is a chronic progressive disease that will lead to joint damage, physical disability and early death.
Studies have shown RA patients due to its inflammatory nature, leads to a higher risk of heart disease or stroke. In the work up of RA, RF is an important test as approximately 70% of patients with RA will have a positive RA. On the other hand, a positive RF does not necessarily mean a person has RA. Clinical features such as symptoms, joint manifestations, and other blood test results have to be taken into account. Another blood test that has a better specificity hence a lower false-positive rate to diagnose RA is anti-CCP – antibody against the cyclic citrullinated peptides.
b) Sero-negative inflammatory arthritis / spondyloarthropathy
Another large component of inflammatory arthritis is known as sero-negative inflammatory arthritis or spondyloarthropathy. The term “spondyloarthropathy” refers to a joint disease of the vertebral column. The types of arthritis that fall into this category are Ankylosing Spondylitis, Psoriatic Arthritis, Inflammatory Bowel Disease-associated arthritis, Reactive Arthritis and undifferentiated Spondyloarthropathy. Although not as prominent, as a whole, the prevalence of this group approximates that of RA.
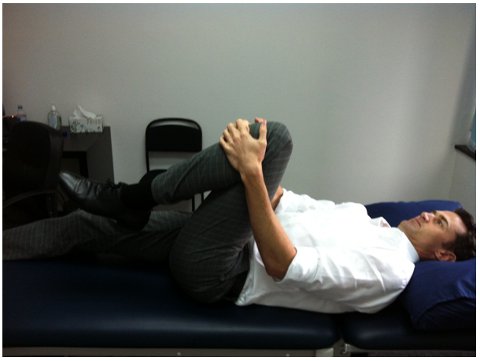
Ankylosing Spondylitis (AS) comprises of inflammation of the sacroiliac joints, spine joints and entheses (point whereby tendon, ligament, joint capsule insert into the bone). One of the commonest presentations of AS is a chronic back pain in a young person (20 to 30 years old). Although the common cause of back pain for this group of people is muscle sprain, the persistent nature over weeks to months and the prolonged stiffness and pain of the back especially in the early morning suggest this inflammation condition. The fact that commonly prescribed anti-inflammatory medications such as NSAIDS work very well for AS patients, some doctors or patients do not recognise that they are dealing with AS till months or years later.
Another subgroup of sero-negative arthritis is psoriatic arthritis which is an inflammatory joint conditions related to psoriasis. Unlike RA, the presentations of joint pain (fingers, wrists, elbows, knees etc) may not be symmetrical but the symptoms are the same – stiffness, swelling, pain. The diagnosis is straight forward if psoriasis of the skin is apparent as most of the time, the clue is from the skin involvement. Other features are the up-lifting of the nail folds from the nail bed (onycholysis), thickened and pitting of the nails and swelling of entire digits (toe or finger) known as dactylitis.
c) Crystals induced arthritis
The commonest condition is gouty arthritis and it is the commonest arthritis in men over 40 years of age although there are sporadic cases in younger men. Premenopausal women seldom develop gout as they are protected from it due to the effects of oestrogen hormone.
However, the prevalence of gout is the same for men and women after postmenopausal age. This arthritis often affects the small joints such as the toes or ankles but can also affect larger joints such as the knees. Occasionally, tophus or collection of deposited uric acid can be seen as nodules on the skin or near the joint. The major risk factor of developing gout is a high blood uric acid levels.
⇒ Related Read: The Secret Hazards of Gout: No Longer a “Rich Man’s Disease”
d) Osteoarthritis
The prevalence of osteoarthritis is higher with age but there are persons under age 40 who developed this condition. This is term secondary osteoarthritis, whereby a previous joint injury such as ligament or meniscus tears, infection or untreated inflammatory arthritis e.g. RA, predisposed the joint to “premature or early failure”.
In osteoarthritis, there are not many features of inflammation such as prolonged stiffness, redness or warmth but there may be swelling and pain. It is important to distinguish osteoarthritis from other inflammatory joint conditions as it will affect the treatment.
e) Soft tissue Rheumatism
Soft tissue rheumatism is not arthritis as the cause of the problem does not arise from the joint itself. Instead, it comprises of inflammation or injury to the tendon, ligament, capsule or muscle leading to symptoms rather similar to arthritis – pain, swelling and stiffness of joints. Examples of soft-tissue rheumatism are muscle sprains, tennis elbow, de quervain tenosynovitis, Achilles tendinitis. Underlying causes are varied ranging from poor postures, overuse syndrome (repetitive strain injury) and worksite ergonomics.
f) Others
Other causes of “rheumatism” pain can be from non-rheumatological or bone condition. These are referred pain from internal organs e.g. gallbladder inflammation leading to the tip of shoulder pain, kidney stones or inflammation of the pancreas leading to back pain or “pins and needles” sensation from the impingement of the nerve mimicking a joint condition. There is also a generalised pain condition known as fibromyalgia which is now known as a central sensitisation syndrome.
Such patients feel pain all over the body when there are no known biochemicals or physiological injury to that part of the body. It may also be associated with fatigue, poor sleep, cognition impairment and depression. It is a challenging problem to treat, often requiring a team of doctors to look into various aspects of the individual.
This article is contributed by Dr Chong Yong Yeow, Specialist in Rheumatology & Consultant, Raffles Internal Medicine Centre, Raffles Medical Group.
* * * * *
Like what you see here? Get parenting tips and stories straight to your inbox! Join our mailing list here.
Want to be heard 👂 and seen 👀 by over 100,000 parents in Singapore? We can help! Leave your contact here and we’ll be in touch.
























































Leave a Comment: