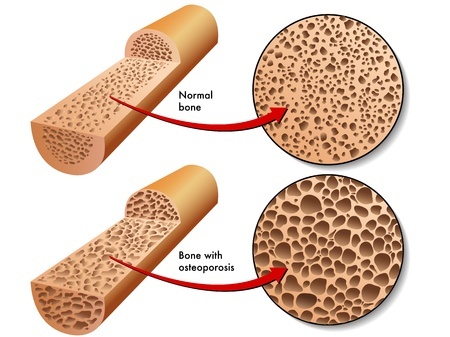
Osteoporosis is characterised by low bone density which decreases bone strength. This condition occurs due to an imbalance between new bone formation and old bone resorption.
Bones start to weaken and become more brittle, as increasing amounts of bone tissues are lost. This places a person with osteoporosis at an increased risk of fragility fractures, commonly in the hip, spine, wrist and shoulders.
Who should be assessed for osteoporosis?
- Women > 65 years
- Post-menopausal/menopausal transition women < 65 years
- Men > 70 years
- Patients with risk factors, as detailed below
What are the risk factors that can contribute to osteoporosis in both men and women?
- Age related bone loss (bone mass will gradually decrease after it reaches its peak in the mid-30s)
- A fracture from “low energy” trauma, for example a hip fracture from a slow and low fall off the bed or chair
- A family history of osteoporosis
- A loss of height or becoming increasingly hunched back
- Inadequate intake of dietary calcium and vitamin D
- Underweight (low body mass index)
- Prolonged bed rest and or low levels of physical activity
- X-rays which suggest thin or brittle bones
- Certain medical conditions, such as liver disease, thyroid disease, rheumatoid arthritis, and malabsorption syndrome
- Some medications, such as steroids and anti-epileptic drugs
- Excessive alcohol intake
- Smoking
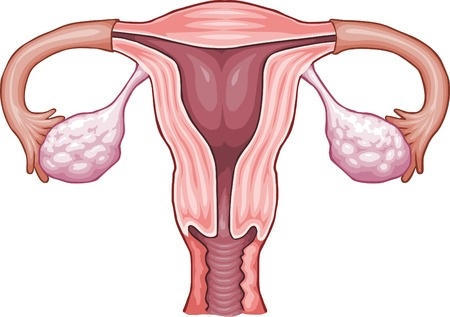
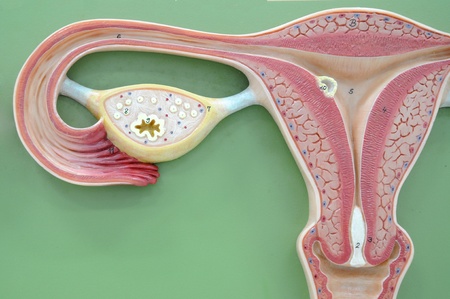
Why are women more susceptible to osteoporosis?
There is a higher tendency for women to develop osteoporosis as they generally have smaller and thinner bones than men. In addition, most women are not as physically active as men, although this trend is changing.
However, the most important cause of osteoporosis in women is menopause. During and after menopause, there is a significant and permanent decrease in oestrogen.
Oestrogen is a female hormone that protects the bones. Decreased oestrogen accelerates the pace of bone loss. Up to 20% of a woman’s bone tissues can be lost in the first 5 years after menopause.
⇒ Related Read: Watch Your Back! Stretching And Lifting Tips For Parents
How can one determine if he or she has osteoporosis?

A bone mineral density (BMD) test can be performed. The most common method is by dual-energy X-ray absorptiometry (DEXA) scan. This scan measures the bone density of your hip and spine, the 2 most common and important areas related to fragility fractures in osteoporosis.
In addition to screening and diagnosis, doing regular DEXA scans allows the doctor to monitor an individual’s bone density results at different intervals to determine if one’s body is responding well to treatment.
What can you do to achieve healthy bones: 5 Things To Note
Adopt good lifestyle habits to keep bones healthy early in life. This is to ensure that maximum bone mass is achieved before it reaches a plateau and starts declining progressively around the age of 35 years.
It is now recommended to start building strong bones during childhood as this will aid in preventing or delaying the onset of osteoporosis later in life.
#1 Maintain a healthy weight and engage in regular outdoor physical exercise to help improve general well-being, muscle strength, postural stability and obtain enough sunlight.

#2 Proper nutrition counts. Consume foods rich in nutrients such as vitamin D and calcium. Examples of food rich in vitamin D include salmon, trout, herring, sardines, egg yolk and mushrooms. As for calcium intake, milk or calcium-fortified soya milk is advised, with the latter being particularly helpful for lactose intolerant patients.
#3 Avoid unhealthy lifestyle habits such as smoking and excessive alcohol intake.
#4 Be extra cautious in order to prevent falls. For example, use non-slip mats and support railings in the bathroom, install adequate lighting (especially at night) and avoid the use of medications that cause drowsiness if possible.
#5 Consult your doctor and go for regular check-ups, especially for those who have risk factors as detailed above.
Are there any treatment or medications available?
Treatment recommendations vary and are based on the individual’s current condition and his/her potential risk of fragility fracture. A useful and free online tool to determine if treatment is needed is the World Health Organization’s Fracture Risk Assessment Tool (FRAX) which calculates the percentage risk of major osteoporosis and hip fractures.
If treatment is needed, there are several medications available. Broadly, these medications can be divided into anti-resorptive or anabolic medications.
An example of anti-resorptive medication is the commonly prescribed bisphosphonates, which slows down the rate of bone resorption and prevents bone loss. Anabolic medications, which take the form of parathyroid hormone injections, can help to stimulate new bone formation and lower the risk of fragility fractures.
These medications, however, have their individual side effects, for example oral bisphosphonates can aggravate existing gastro-oesophageal reflux and are contra-indicated in patients with renal impairment.
It is recommended that you should always seek medical advice from your health care provider to determine the best treatment option for you.
This article is written Dr Leon Foo, a Consultant Orthopaedic Surgeon from the Island Orthopaedic Consultants Pte Ltd, a member of Healthway Medical Group. Dr Foo has special interest in hip, knee and shoulder problems, sports injuries, arthritis, bone & soft tissue tumours.
* * * * *
Like what you see here? Get parenting tips and stories straight to your inbox! Join our mailing list here.
Want to be heard 👂 and seen 👀 by over 100,000 parents in Singapore? We can help! Leave your contact here and we’ll be in touch.