Recognising these serious accidents or conditions that happen in babies and young children can be tough. We asked a doctor how to recognise signs of life-threatening conditions and tips on how to prevent them from happening.
If you notice any of the problems listed below, seek medical attention as soon as possible.
1. Choking
This is very common and preventable. A piece of food or a small toy/object gets lodged in the baby’s/child’s airway, causing airway obstruction. It can occur very suddenly when the child picks up the food/object and places it in the mouth.
Choking risks include:
i. Food items e.g. whole peanuts, lollies, grapes, seeds, pieces of meat etc
ii. Household items e.g. coins, small batteries, small magnets, the caps of pens and markers, and jewellery
iii. Toys and toy parts e.g. plastic shapes, marbles, eyes of stuffed toys, table tennis balls and balloons (uninflated or popped)
iv. Garden objects e.g. pebbles
v. Any other small items
Tips for preventing choking

i. Sit while eating
ii. Encourage your child to chew food well
iii. Keep food pieces small
iv. Avoid nuts or seeds
v. Cook, grate or mash hard foods e.g. carrots and apples
vi. Try to keep small objects out of reach
vii. Use toys that are solid and sturdy. Avoid toys with small parts, breakable parts or brittle surfaces. Check toys for exposed stuffing, loose screws and buttons. Avoid buying toys with button batteries.
viii. Keep toys for small children and older siblings in separate boxes. Small toys should be kept out of reach from young children e.g. Lego, doll clothes, beads, car parts etc.
When choking happens, call for help immediately and first aid will be required urgently. For specific details on the first aid measures required, please refer to Health Topics A to Z on the Kids Clinic website: “Throat Problems: Child Choking”
2. Respiratory failure/severe respiratory distress
E.g. severe pneumonia, severe bronchiolitis/bronchitis, severe asthma etc.
This refers to severe breathing difficulties due to airway/lung problems, with poor intake of oxygen and poor removal of carbon dioxide from the body, which can result in failure of multiple organs.
Signs observed may include fast breathing, shallow breathing, in-drawing of skin over the ribcage, grunting, excessive usage of abdominal muscles or neck muscles during breathing, audible noisy breathing coming from the chest region, lethargy/drowsiness, abnormal skin colour etc.
Seeking urgent medical attention is of paramount importance because specific treatment can then be given quickly, such as oxygen, nebuliser, antibiotics etc. Some cases may even require breathing support urgently.
3. Sudden Infant Death Syndrome (SIDS)

Sudden infant death syndrome (SIDS) is the unexplained death, usually during sleep, of a seemingly healthy baby less than a year old. SIDS is sometimes known as crib death because the infants often die in their cribs.
Risk factors for SIDS
i. Sex. Boys are slightly more likely to die of SIDS.
ii. Age. Infants are most vulnerable between the second and fourth months of life.
iii. Race. For reasons that are not well understood, non-white infants are more likely to develop SIDS.
iv. Family history. Babies who have had siblings or cousins die of SIDS are at higher risk of SIDS.
v. Secondhand smoke. Babies who live with smokers have a higher risk of SIDS.
vi. Being premature. Both being born early and having a low birth weight increase your baby’s chances of SIDS.
vii. During pregnancy, the mother also affects her baby’s risk of SIDS, especially if she:
- Is younger than 20
- Smokes cigarettes
- Uses drugs or alcohol
- Has inadequate prenatal care
Prevention
- Back to sleep
Place your baby to sleep on his or her back, rather than on the stomach or side, every time you – or anyone else – puts the baby to sleep for the first year of life. This is not necessary when your baby is awake or able to roll over both ways without help.
Don’t assume that others will place your baby to sleep in the correct position – insist on it. Advise sitters and child-care providers not to use the stomach position to calm an upset baby.
- Keep the crib as bare as possible
Use a firm mattress and avoid placing your baby on thick, fluffy padding, such as lambskin or a thick quilt. Don’t leave pillows, fluffy toys or stuffed animals in the crib. These can interfere with breathing if your baby’s face presses against them.
- Do not overheat your baby
To keep your baby warm, try a sleep sack or other sleep clothing that doesn’t require additional covers. Do not cover your baby’s head.
- Have your baby sleep in your room
Ideally, your baby should sleep in your room with you, but alone in a crib, bassinet or other structure designed for infants, for at least six months, and, if possible, up to a year. Adult beds are not safe for infants.
A baby can become trapped and suffocate between the headboard slats, the space between the mattress and the bed frame, or the space between the mattress and the wall. A baby can also suffocate if a sleeping parent accidentally rolls over and covers the baby’s nose and mouth.
- Breast-feed your baby
If possible. Breast-feeding for at least 6 months lowers the risk of SIDS.
- Do not use baby monitors and other commercial devices that claim to reduce the risk of SIDS
The American Academy of Paediatrics discourages the use of monitors and other devices because of their inefficacy and safety issues.
- Offer a pacifier

Sucking on a pacifier without a strap or string at naptime and bedtime might reduce the risk of SIDS. One caveat — if you are breast-feeding, wait to offer a pacifier until your baby is 3 to 4 weeks old and you have settled into a nursing routine.
If your baby is not interested in the pacifier, do not force it. Try again another day. If the pacifier falls out of your baby’s mouth while he or she is sleeping, do not pop it back in.
- Immunise your baby
Some evidence indicate that immunisations can help prevent SIDS.
4. Multiple trauma (e.g. from Road Traffic Accidents)
This refers to trauma to multiple areas of the body, which could be accidental (e.g. from road traffic accidents, unwitnessed falls etc.) or non-accidental (e.g. from child abuse).
Common consequences from multiple trauma which may result in death include excessive bleeding, severe head injury, severe trauma to solid organs etc.
Specifically, to reduce the risk of child injuries in a road traffic accident, the following are the recommendations for car seating from the American Academy of Paediatrics:
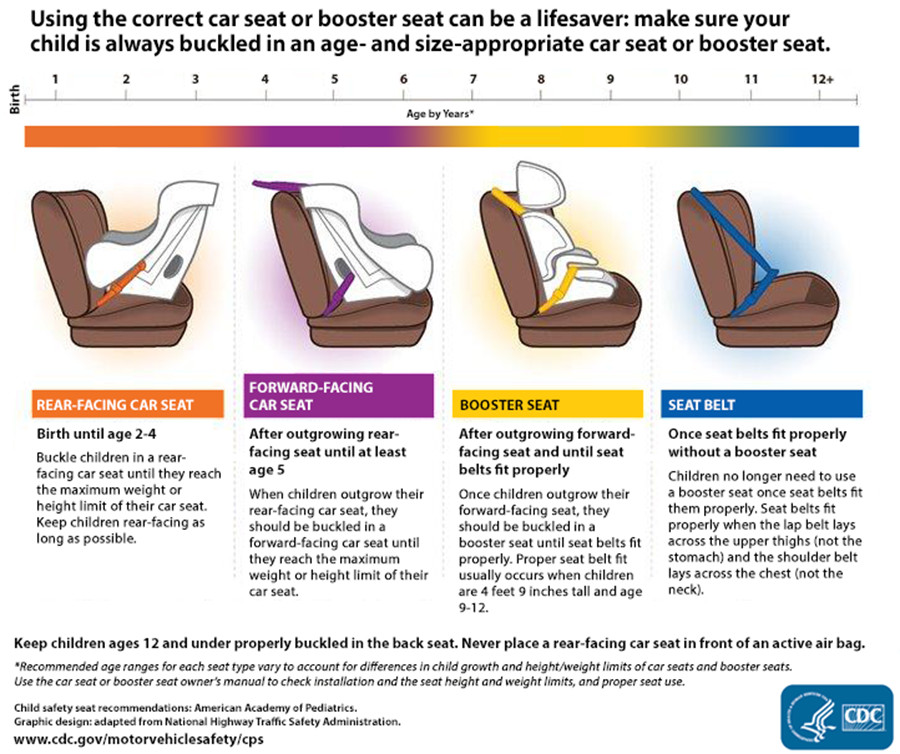
Click here for a larger view. Image source: American Academy of Paediatrics
Other important measures
- Do Not Seat Children in Front of an Airbag
Airbags can kill young children riding in the front seat. Never place a rear-facing car seat in front of an air bag.
- Seat Children in the Back Seat
Buckle all children aged 12 and under in the back seat.
- Seat Children in the Middle of the Back Seat
Buckle children in the middle of the back seat when possible, because it is the safest spot in the vehicle.
- Use Proper Restraints Every Trip
Buckle children in car seats, booster seats, or seat belts on every trip, no matter how short.
- Parents and Caregivers: Always Wear a Seat Belt
Set a good example by always using a seat belt themselves.
5. Sepsis
This is an overwhelming infection (typically by bacteria), which causes multiple organs in the body to fail.
The presenting symptoms can be fairly non-specific, e.g. fever, lethargy, poor feeding, vomiting, drowsiness/irritability, shortness of breath, poor skin colour etc, which can sometimes resemble common conditions such as simple stomach flu or a cold initially (especially in the early stages when symptoms are still evolving).
The important point here is early identification of sepsis by your child’s doctor, especially when fever is persistent or if your child becomes sicker despite initial medications/treatment. Hence, it is prudent to seek medical attention early.
Appropriate early initiation of antibiotics for a suspected bacteria infection can help to treat the specific infection and reduce the risk of sepsis developing.
6. Severe Dehydration
In this preventable condition, there is a marked reduction in total body water content, with loss of important salts (such as sodium and potassium), resulting in circulatory shock and end organ dysfunction.
It can occur when there is reduced oral fluid intake from poor feeding and loss of fluids/salts through vomiting, diarrhoea, excessive sweating etc.
The presenting symptoms include reduced urine output, dry tongue/lips, lack of tears when crying, sunken eyes, abnormal skin turgor, lethargy/drowsiness etc.
Early initiation of oral hydration with appropriate fluids containing sugar and salts is very important, and should be started even before dehydration sets in.
It is also important to manage ongoing vomiting and/or diarrhoea with appropriate medications, in order to reduce loss of fluids/salts.
In cases where the child is very dehydrated, hospitalisation with early initiation of intravenous (IV) fluids will be of paramount importance to reverse the effects of dehydration.
7. Acute Myocarditis
This involves inflammation/infection of the cardiac (heart) muscles, resulting in cardiac dysfunction, circulatory shock and abnormal heart rhythm. It can begin from what seems like a simple cold or stomach flu.
It is not easy to diagnose and requires a high index of suspicion because the symptoms can be very non-specific at the start, including poor feeding, vomiting, abdominal pain, chest pain, breathlessness, lethargy etc, which may resemble other more common childhood conditions.
The key is in early suspicion and identification, with escalation of care to a tertiary paediatric centre that is able to manage such cases, because very often they require infusion of medications to support the heart function and blood pressure, and may even require a heart-lung machine when the condition worsens.
8. Cardiac Arrhythmias (e.g. supraventricular tachycardia, SVT)

This is an abnormal heart rhythm, which compromises the function of the heart and can result in a sudden collapse of the baby/child.
Older children or teenagers may report abnormal heartbeat (i.e. palpitations), chest pain, shortness of breath, giddiness etc. However, younger children and babies may only have non-specific symptoms such as poor feeding, vomiting, looking pale etc.
Once suspected, a heart rhythm strip (ECG) should be done to assess the heart rhythm properly, with the appropriate management for the specific cardiac arrhythmia subsequently.
In cases where the baby/child has collapsed, cardiopulmonary resuscitation (CPR) and defibrillation (via an automated external defibrillator, AED) will be required urgently, while awaiting escalation of care to a tertiary paediatric centre (if not already in one).
Babies/children, whose family members have a history of arrhythmias, early cardiac diseases or sudden cardiac deaths, may be at higher risk of such cardiac arrhythmias.
This article is written by Dr Dave Ong, a paediatrician with special interests in allergies, skin conditions and respiratory problems in children. He also has a keen interest in the management of acute infections in children, newborn care and development, feeding problems, and vaccinations.
He is currently practising at Kids Clinic @ Punggol (Oasis Terraces #03-11) which is also open on selected weeknights and Sundays.
* * * * *
Like what you see here? Get parenting tips and stories straight to your inbox! Join our mailing list here.
Want to be heard 👂 and seen 👀 by over 100,000 parents in Singapore? We can help! Leave your contact here and we’ll be in touch.






















































Leave a Comment: