Does my child’s walking seem odd? Why is my son tripping frequently?
My daughter seems to be developing bunions but she’s only 7, how can that be?

These are all questions we podiatrists frequently encounter during clinical consultation with anxious parents. As parents, you are worried for your children’s health.
Learning more about paediatric foot conditions can help to alleviate parental concerns and educate you on making the right choices for your child’s care.
Here are five common paediatric foot conditions to look out for.
1. Flat Foot

Known as a pes planus deformity, flat foot can occur in one foot or both feet. Flat foot is normal in infants and young children, and in most cases, the child’s foot will develop an arch over time.
While having a flat foot or low arches does not automatically mean that the child requires treatment, flat feet can place additional strain on certain structures of the foot and lower limbs, causing discomfort or other symptoms. Here are several ways to identify flat foot.
Wet Footprint Test
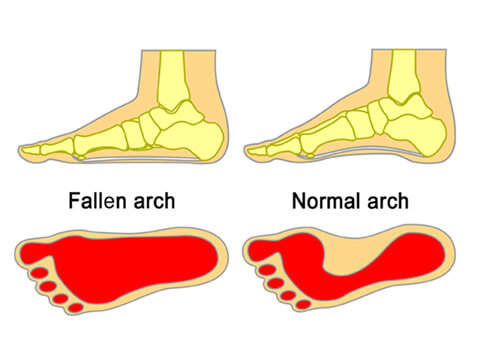
Wet your child’s feet and have them stand on a surface that will clearly show their footprint, such as concrete, before stepping away.
If you do not see a normal arch shape and the print of your child’s whole foot resembles the fallen arch, it is likely that they have a low arch or flat foot.
Footwear Evaluation
Examine the wear patterns on your child’s footwear. Pay particular attention to the inside of the sole and the area around the heel, as these areas will experience increased wear and tear if your child has flat foot.
Tiptoe test
If your child appears to have little or no arch when standing, have them tiptoe. In some cases, the arch of the foot will appear. Known as flexible flat feet, this usually has fewer complications than regular flat foot.
Treatment
In many cases, flat foot does not require any treatment. However, if your child is experiencing pain in their feet, particularly around the heel and arches, or discomfort while standing, walking or running, you may consult a podiatrist to ensure that there are no underlying conditions responsible for the discomfort.
Treatment options will vary depending on the diagnosis, but will focus on reducing discomfort, healing injured tissue and preventing the recurrence of the issue.
Depending on the child’s age and condition, treatment options may include steroid injections, physical therapy, shockwave therapy, prescribed insoles or braces, and surgery in complex cases.
2. In-toeing and Out-toeing

Both of these conditions are related to the alignment of the child’s foot. In-toeing, also known as pigeon toe, occurs when a child’s feet turns inward instead of pointing straight ahead.
Out-toeing occurs when a child’s foot turns outwards rather than pointing straight ahead. In-toeing and out-toeing are both normal during a child’s growth and will typically correct themselves over time.
Possible causes for In-toeing
- Femoral anteversion (thigh bone is turned inwards)
- Internal tibial torsion (shin or lower leg is turned inwards)
- Metatarsus Adductus (forefoot is curved inwards)
Possible causes for Out-toeing

- Femoral retroversion (thigh bone is twisted outwards)
- External tibial torsion (shin or lower leg is turned outwards)
- Cerebral palsy (damage to the brain that affects muscle and movement)
Symptoms of Pigeon toeing
- visibly inward facing forefeet
- very curved feet that are shaped like crescents
Symptoms of Out-toeing
- visibly outward facing feet
Symptoms that are common to both conditions include limping, swelling, and frequent tripping or excessive clumsiness. If your child appears to be visibly in-toeing or out-toeing and experiences pain, consult a specialist of the foot immediately to ensure that it is not related to a more serious condition.
Treatment
While treatment will depend on the diagnosis and the specifics of a child, a typical treatment plan for these conditions can include orthotics such as custom insoles, braces or casts. In more severe cases, surgery may be the only option to address the issue.
3. Juvenile Bunions

Bunions, also known as hallux valgus, are a bony deformity that is usually characterised by a bulge or swelling near the base of the big toe. It is a very common condition and research suggests up to half the adult population develops bunions.
Bunions can develop from a young age, with the average age for juvenile cases occurring between seven to ten years old. Many assume that bunions are caused by poor fitting or uncomfortable footwear, particularly high heels.
However, research has found that hereditary factors, particularly from the mother, are the biggest reason for children developing bunions.
Risk factors
- Moderate or severe flat foot
- Joint hypermobility
- Genetics
Symptoms
- Pain and difficulty finding suitable shoes
- Impaired movement
- Swelling and/or pain at the base of the big toe.
Treatment
The key to treating bunions is to remember that it is a progressive disease. This means that the condition will worsen over time, becoming harder and more complex to treat.
Early treatment options include bunion splints, which can be worn overnight to secure the joint; sports tape, which can be used to temporarily correct the joint; and customised orthotic insoles, which can reduce pressure and correct the joint.

If the condition worsens sufficiently, surgery may be the only option. This is less commonly recommended for juveniles as they have not reached skeletal maturity, and should only be considered if the quality of life of the child is severely impaired.
3. Verruca Warts

Warts are small rough growths or lumps growing on the skin that are caused by the Human Papilloma Virus (HPV). While warts are typically harmless and may go away on their own, verrucas can be painful as they are located on the bottom of the foot.
Pressure is placed on the wart when we are on our feet, causing pain and discomfort. To reduce the discomfort, some patients make changes to their gait or posture, potentially straining or causing discomfort in other parts of their body.
Symptoms
- Lump that resembles a cauliflower
- Rough hard skin on the sole
- Tiny black dot under the skin
- Painful when squeezed
Prevention
As verrucas are spread through skin contact or contact with HPV, there are several things you can do to help reduce the chance of your child coming into contact with the virus.
- Avoid going barefoot in wet areas such as communal pools or showers
- Remind your child not to share their towels, shoes and socks
- Avoid picking at or scratching existing warts and verrucas
Treatment
In some cases, it may be advised for the verruca to be left alone. If it is causing discomfort or affecting your child’s quality of life, the clinician is likely to propose treatment.
This can include cryotherapy, where the wart is frozen, applying salicylic acid or silver nitrate to the verruca to remove the infected tissue, and surgical removal of the wart. Regardless of the method, several sessions are often required to ensure successful removal of the verruca.
This article is contributed by Ari Tria, a Senior Podiatrist practicing at East Coast Podiatry‘s Kembangan branch. Ari is experienced in both public and private health settings and has practiced in several countries. She enjoys working with children and her clinical specialities lie in diabetic foot care and paediatric foot conditions.
Images by East Coast Podiatry.
* * * * *
Like what you see here? Get parenting tips and stories straight to your inbox! Join our mailing list here.
Want to be heard 👂 and seen 👀 by over 100,000 parents in Singapore? We can help! Leave your contact here and we’ll be in touch.





















































Leave a Comment: